Why Are Jews At Higher Risk For Pancreatic Cancer?

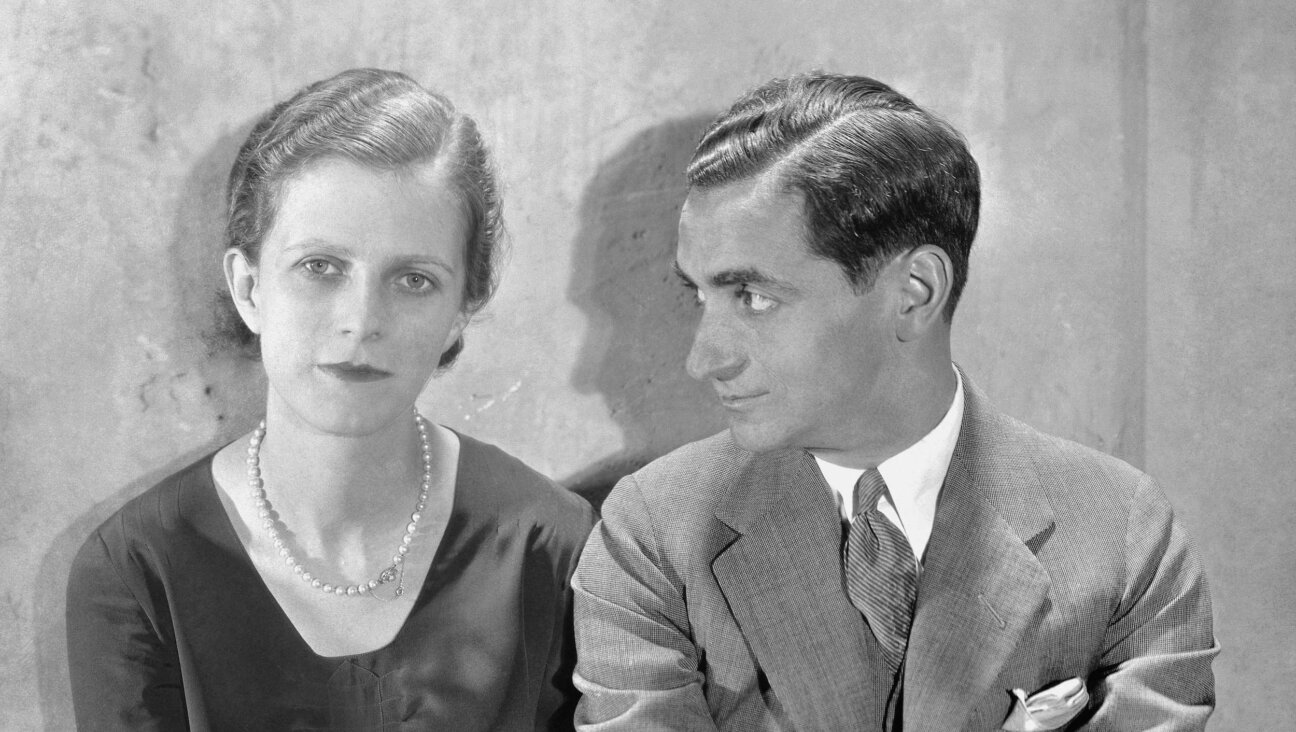
Justice Ruth Bader Ginsburg. Image by Getty Images
Ruth Bader Ginsburg is a rarity in more ways than one. She is not only the first Jewish woman to serve as a Supreme Court Justice, but also one of the few survivors of pancreatic cancer. In February 2009, a small tumor in Ginsburg’s pancreas was removed, and reportedly it has not returned since — remarkable for a disease which has a five-year survival rate between 1 and 14%.
According to the American Cancer Society, pancreatic cancer, though relatively uncommon, is fourth among the leading causes of cancer deaths this year, just behind lung, prostate/breast, and colon/rectal cancers. Within a few decades, pancreatic cancer is expected to rise to the second cause of cancer deaths, mostly because an aging population is more likely to be diagnosed. There are currently no early detection tests for pancreatic cancer, and physical symptoms — which include jaundice, unexplained weight loss and abdominal or back pain — appear only after the cancer has grown throughout or beyond the pancreas and can no longer be successfully treated. About 1 in 40 Jews in the United States will get pancreatic cancer, compared to 1 in 67 in the overall U.S. population, according to a 2011 study published in the journal Cancer Epidemiology, Biomarkers & Prevention. The reasons for this higher risk are not yet known. An ongoing study at Yale University could shed light on other genetic risk factors and open up avenues for early screenings.
Pancreatic cancer runs in families, and approximately 10% of all cases occur in individuals with a genetic predisposition for the disease. BRCA mutations, which are well known risk factors for breast and ovarian cancer and occur at a higher rate among Ashkenazi Jews, can also increase the risk of pancreatic and prostate cancer, albeit to a lesser degree. People with these mutations have a two- to six-fold increased risk of developing pancreatic cancer over general population estimates, though data is limited.

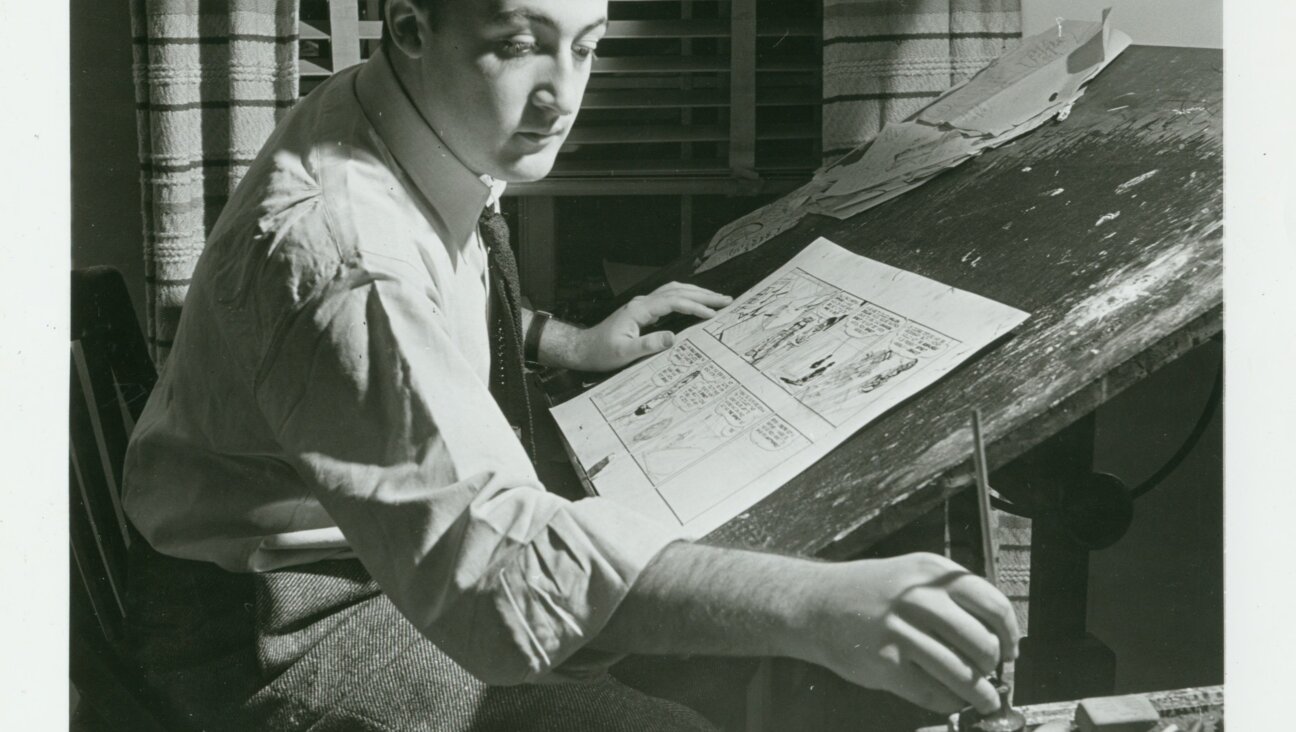
Exploring Family Histories: Dr. Aimee L. Lucas authored a study which showed that people with a family history of pancreatic cancer frequently have BRCA mutations. Image by Courtesy of Aimee L. Lucas
On the other hand, Ashkenazi Jews with pancreatic cancer have also been found to have a higher than expected prevalence of BRCA mutations, a study published this year in the journal Cancer showed. The research also showed that individuals who have a family history of pancreatic cancer are frequently found to have these genetic mutations. “At this point, we do not fully understand which patients who carry the BRCA1 or BRCA2 mutations are at risk for pancreatic cancer,” said Aimee L. Lucas, assistant professor of medicine and gastroenterology at the Icahn School of Medicine at Mount Sinai, in New York, and lead author of the study. Knowing who has a family history of pancreatic cancer, along with the genetic markers, can help identify people who should undergo regular screenings. This may lead to earlier diagnosis and treatment of pancreatic tumors, which could ultimately lead to higher survival rates.
The first study to determine which other genetic factors — apart from the BRCA mutations — put Jews at higher risk of developing pancreatic cancer is currently underway at Yale University. Yale professor Harvey Risch and Ph.D. student Samantha Streicher are analyzing anonymous genetic research data stored in repositories of the National Institutes of Health, and will complete their study in 2015. “The overall goal of our research is to have a better understanding of the increased risk of pancreatic cancer in Jews,” said Streicher. “I hope it will significantly add to the field of pancreatic cancer research and that progress is made toward better prevention and treatment of the disease.”
For the National Familial Pancreas Tumor Registry at Johns Hopkins University, the leading organization that tracks family histories of pancreatic cancer, Ashkenazi Jewish families provide vital clues to understanding the disease. “Since pancreatic cancer is more common in individuals of Jewish descent than it is in the general population, it could be due to an inherited factor, an environmental factor, or due to chance,” said Dr. Ralph H. Hruban, director of the Sol Goldman Pancreatic Cancer Research Center at The Johns Hopkins University School of Medicine. “By collecting information on family history and on environmental exposures, we can identify the causes for the higher rate of pancreatic cancer, and in so doing, hopefully offer some hope to those impacted.”
The family patterns typically seen among Ashkenazi Jews are a particularly compelling factor in this research. “Because individuals of Ashkenazi Jewish heritage tend to marry other individuals of Ashkenazi Jewish heritage, there is less genetic diversity in the Ashkenazi Jewish population,” said Hruban. “This means that it can be easier for us to discover the genetic causes in this population as there is less ‘background noise’ in our genetic studies.” Scientists have already discovered several genetic mutations that cause about 15% of the familial clustering of pancreatic cancer. Pinning down genetic risk factors is important because it opens up possibilities for screening for early tumors in the pancreas. “In the research setting, we have shown that asymptomatic early tumors can be detected in some of these people,” said Hruban. “We believe this is a first step toward developing an early detection test for pancreatic cancer. Just as colonoscopy saves lives by detecting early curable colon polyps, so too do we want to save lives by detecting early curable tumors of the pancreas.”
While screenings for breast and prostate cancer are universally encouraged, pancreatic cancer screenings are not currently recommended for the general population. “Screening for a disease is useful if either the disease is relatively common or the screening test is virtually perfect,” said Risch. There are a high number of false positives with pancreatic cancer screens, due to the overall rarity of pancreatic cancer and because current screening measures aren’t 100 percent accurate all the time. As a result, they can cause unneeded stress and costs for follow-up care.
The importance of early detection becomes apparent in Ginsburg’s case. She had been successfully treated for colon cancer a decade earlier, and then in 2009 doctors found a one-centimeter long tumor in the middle of her pancreas — during a routine CT scan. It was the smallest tumor that could have been detected that way.
For those who have no reason to undergo routine scans, making healthy lifestyle choices remains one strategy to reduce risk: For both Jews and non-Jews, not smoking and maintaining a healthy weight are vital to not only lowering the risk of developing pancreatic cancer, but avoiding other types of cancer as well.
Cheryl Alkon is a longtime health writer; her work has appeared in USA Today, USA Weekend, Boston magazine, and more. She is the author of Balancing Pregnancy With Pre-Existing Diabetes: Healthy Mom, Healthy Baby. Find out more at CherylAlkon.com.