Genetic Testing For Sephardic Jews Faces Reluctant Community

Breaking Taboo; Dr. William Warren Brien (left), former mayor of Beverly Hills, at the annual Neuromuscular Disease Foundation Gala with Carolyn Yashari Becher, executive director of NDF, which funds HIBM research and seeks to raise awareness about genetic disease in Sephardic communities. Image by Neuromuscular Disease Foundation
When Jennifer was 26, people started asking her why she was limping. An exercise enthusiast, she brushed aside the question. Then she noticed she couldn’t run laps in her kickboxing class. No problem, she thought — running wasn’t her thing. Next, she started falling behind some older women in Pilates class. By that time, she and her husband were planning on starting a family. Just to be safe, she decided to see a doctor.
Jennifer, a psychiatrist who asked that only her first name be published because she does not want her personal story revealed to patients, first saw a sports physician. He referred her to a podiatrist, who advocated surgery. Unwilling, she went to a physical therapist.
“You definitely have weakness,” she remembers him saying about her muscles. Though he didn’t think it was anything serious (“not genetic or progressive”), he sent her to a neurologist at UCLA. The medical fellow who examined her was a Persian Jew. He knew exactly what was wrong — it was genetic, and it was definitely progressive.
Jennifer has hereditary inclusion body myopathy, a rare, recessive genetic disease that causes late-onset muscle degeneration. The carrier rate in the Persian Jewish community is 1 in 15 — more common than Tay-Sachs is for Ashkenazi Jews. Cases of HIBM have also been documented among non-Jews, including Japanese, Caucasian Americans, Asian Indians and Kurdish Iranians.
Until recently, Jewish genetic diseases have been largely linked with Ashkenazi Jews, amongst whom aggressive prenatal genetic testing has effectively eradicated devastating conditions such as Tay-Sachs.
Now, as the first generation of American-born Jews from Iran and other Middle Eastern countries comes of age, research is turning to diseases in their communities, which have not had the same institutional organizations as the Ashkenazim.
“I had never even heard of [HIBM],” said Jennifer, whose family came to the United States from Iran nearly 50 years ago. “It’s pretty emotionally traumatic to be standing in a room and hear someone tell you that. It shatters your world and everything your life is set out to be.”
Because of its high carrier frequency and appearance in a person’s mid-20s or early 30s, HIBM, of all the genetic diseases suffered by Jews from the Middle East, has gotten the most attention in the United States. Some hope it will be a model for implementing prenatal screening in a community where genetic disease is often misunderstood or carries a heavy stigma.
Because there is no cure or treatment for HIBM, potential carriers are reluctant to get tested, knowing the outcome is eventually the loss of important muscle function and a wheelchair-bound existence. “You know what’s coming, and in that moment you know there’s nothing you can do to stop it,” Jennifer, now 38 and a mother of two children, said about the disease. “With HIBM, you are constantly having to mourn new losses and look ahead at the future. You can’t ever fully mourn it because it’s always changing.”
A recently launched clinical trial by Ultragenyx Pharmaceutical may offer light at the end of what is now a very dark tunnel. The Ultragenyx trial is a double-blind study of 46 participants, testing the potential of sialic acid on muscle activity. Though the study, conducted in coordination with experts in Japan and Israel, is still in the second stage of a three-phase trial, an interim analysis after 24 weeks showed some improvement in muscle strength, particularly in the upper extremities. No changes were noted in the lower extremities.
“The reality of it is that these things are developments,” explained John Ditton, vice president at Ultragenyx. “What we’re trying to do with HIBM is say ‘Let’s put one foot forward here.’”
Still, the best bet for eradicating the disease remains genetic counseling and prenatal screening, which allow carriers and affected people options and awareness.
Several large medical institutions — one in Israel, one in Los Angeles and one in New York — offer prenatal testing for HIBM and certain other so-called Sephardic or Mizrachi Jewish genetic diseases. Prior to 2010, any tests for HIBM had to be sent to Hadassah Hospital in Israel, where Dr. Zohar Argov first identified the condition. Later, together with Dr. Stella Mitrani-Rosenbaum, Argov also identified the specific gene mutation that caused the condition.
Argov discovered the disease by chance in 1979, when as a young doctor he saw a patient who supposedly had muscular dystrophy. He found the man in a wheelchair, with his granddaughter sitting on his extended legs — an unlikely position for someone with that condition. Intrigued, Argov started hunting for similar cases. “The more I looked, the more I found. I noted that more and more of these people have this unique phenomenon and they’re all Persian Jews.”
In 1994 he joined forces with Mitrani-Rosenbaum, and in 2001 her lab discovered the gene mutations causing the condition. Then, Argov noted something peculiar: Researchers in other countries had documented similar cases, without connecting the dots. “It turned out that it’s not unique to Persian Jews,” he said. “It exists worldwide with other mutations.”
In 2006, Jennifer’s mother founded the Neuromuscular Disease Foundation to raise awareness of HIBM and fund research. In 2012, the foundation gave $200,000, raised through its annual gala, to Argov and Mitrani-Rosenbaum’s lab.
Yet comprehensive screening for the disease has been slow in coming. In 2009, Cedars-Sinai Hospital in Los Angeles launched a pilot program to test people for four recessive diseases that are found at elevated frequencies among Jews from Iran.
“L.A. has a huge Persian Jewish community, so the need for that type of panel was great and we wanted to fill that hole,” said Catherine Quindipan, the genetic counselor in charge of the project.
From the results obtained by testing 1,000 people over two years, Cedars-Sinai was able to launch a Persian Jewish genetic panel in 2011, which enables prenatal screening for HIBM, pseudocholinesterase deficiency, polyglandular deficiency and congenital hydrocephalus — the four main genetic conditions prevalent among that population.
Similar panels are available in the New York area. In 2009, Dr. Martin Bialer of North Shore University Hospital in Long Island started developing a panel to screen for HIBM and Wolman disease, two conditions, he reasoned, that would have the most impact on couples thinking about starting a family.
“What we looked out for was, ‘What conditions does it make sense to screen for in a pregnant woman?’” he said.
Armed with their genetic status, carriers who want children have options. Randi Zinberg, a genetic counselor at Mount Sinai Hospital in New York, laid out three. A couple can choose to do nothing and take their chances — in the case of HIBM, the child will have a 1 in 4 chance of inheriting the condition if both parents are carriers. The second option is a prenatal diagnosis through chorionic villus sampling (done as early as 10 weeks), or amniocentesis (done from 15 weeks on). Early testing offers parents the options of terminating the pregnancy, or at the very least getting their options reviewed by a genetic counselor or physician. Finally, they can choose to use preimplantation genetic diagnosis, which tests the embryos for mutations prior to in-vitro fertilization, or gamete donation (sperm or egg).
Mount Sinai Hospital has developed a similar panel. But Ruth Kornreich, associate professor in genetics and genomic sciences, has broader plans. “We are currently working to expand our Jewish genetic disease panel, which would include both Ashkenazi and Sephardic Jewish mutations,” she explained, by which she meant mutations experienced by Jews from the Middle East.
But there is a special difficulty in developing an overarching panel for Jews from the Middle East. Unlike Ashkenazi Jews, who form a fairly unified transnational gene pool, Jews from the Middle East — Iranian Jews, Ethiopian Jews and Moroccan Jews, to name a few — each have their own discrete genetic diseases.
“For example, it might not make sense to screen for HIBM in a different [non-Iranian] subgroup,” Kornreich explained. This makes it harder to develop all-encompassing genetic tests similar to those tests now used for the Ashkenazi population.
Mount Sinai is currently determining the carrier frequencies for each disease, attributing them to relevant subgroups and validating the methodologies. The hospital hopes to have the expanded panel ready this year.
But the main barrier to screening remains the stigma that various populations of Jews from the Middle East attach to genetic disease.
In 2010, Dr. Gidon Akler, a fellow in the genetics and genomic sciences department at Mount Sinai and a colleague of Kornreich, co-founded the Sephardic Health Organization for Referral and Education with Bob Kamali, a prominent member of the New York-based Persian Jewish community who lost his 6-month-old granddaughter to Wolman disease. Their goal was to create a website that would disseminate information about genetic conditions associated with subgroups of Jews from the Middle East.
One of Akler’s first goals for SHORE was to coordinate with the Jewish Genetic Diseases Consortium, the alliance of not-for-profit organizations at the forefront of raising awareness about genetic disease in the Ashkenazi community. In 2010, Akler, a JGDC board member, consulted with Randy Yudenfriend Glaser, chair of the board, to have 17 “Sephardic/Mizrahi Jewish Genetic Diseases” added to the list of 20 “Ashkenazi Jewish Diseases.”
But even with this nominal change, Yudenfriend Glaser noted that providing the same sort of education and outreach offered in the Ashkenazi community has been a challenge.
“It has been very difficult to integrate into the Sephardic community even with people helping us,” she said.
In L.A., Quindipan described a similar barrier. “There is an immense [stigma] to being found that you’re a carrier of a genetic condition because there’s a fear that it can affect the marriage prospects of people from that family,” she said.
Cedars-Sinai has been coordinating with local rabbis, community centers and grassroots organizations like the Neuromuscular Disease Foundation, founded by Jennifer’s mother, and Advancement for Research Myopathies — founded by Drs. Daniel and Babak Darvish, two brothers diagnosed with HIBM — to help get the word out, but progress has been slow.
“People will say they have [multiple sclerosis], they’ve had a car accident, all kinds of stories — anything to cover up the fact that this is something genetic,” explained Carolyn Yashari Becher, Jennifer’s sister, who took over as executive director of NDF after their mother retired. “People want to get their children married before anybody finds out. One of the ways we’re trying to push this is through the rabbinic community and say you cannot marry people without encouraging them to get tested.”
In Israel, intermarriage between Sephardic and Ashkenazi Jews, and widespread awareness campaigns, have made headway into traditionally insular communities to promote the importance of genetic testing.
“Somehow Ashkenazi Jews took their diseases as a normal thing for their community. I suppose there was stigma but with time people got used to the idea,” explained Dr. Ohad Birk, head of the Center for Human Genetics Research at the National Institute for Biotechnology in Israel. “I’ve been a physician in Israel for 30 years and I’ve not seen a single case of Tay-Sachs. The reason is that the prevention system works. And that’s the true answer: not to hide from these problems, rather tackle them and prevent them.”
Yashari Becher stressed that the negative associations are slowly fading as people like Jennifer come forward.
“My sister was one of the first people ever to get up and speak publicly about having this disease,” she said. “Through that, she has really broken down a lot of the stigma because what she has done is put a face to this disease and really brought it home for people. What we have done is really pushed the statistics and said ‘Look these people are in our communities, they are in our families, we cannot ignore this any longer.’”
Contact Anne Cohen at [email protected]
The Forward is free to read, but it isn’t free to produce

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward.
Now more than ever, American Jews need independent news they can trust, with reporting driven by truth, not ideology. We serve you, not any ideological agenda.
At a time when other newsrooms are closing or cutting back, the Forward has removed its paywall and invested additional resources to report on the ground from Israel and around the U.S. on the impact of the war, rising antisemitism and polarized discourse.
This is a great time to support independent Jewish journalism you rely on. Make a gift today!
— Rachel Fishman Feddersen, Publisher and CEO
Support our mission to tell the Jewish story fully and fairly.
Most Popular
- 1

Fast Forward Ye debuts ‘Heil Hitler’ music video that includes a sample of a Hitler speech
- 2

Opinion It looks like Israel totally underestimated Trump
- 3

Culture Cardinals are Catholic, not Jewish — so why do they all wear yarmulkes?
- 4
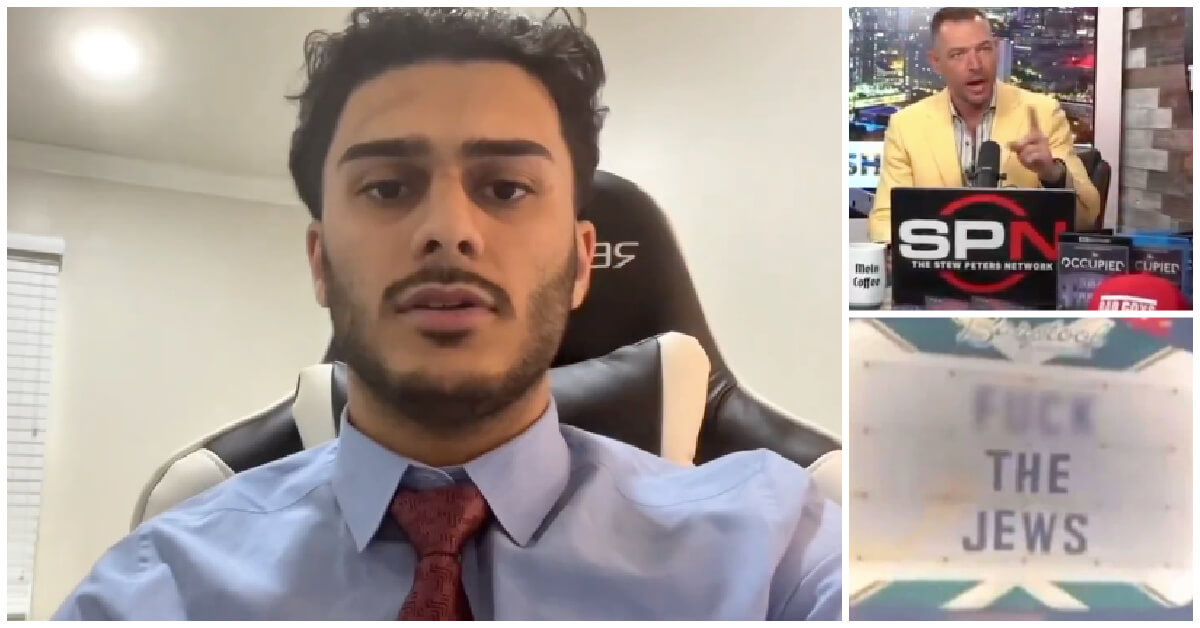
Fast Forward Student suspended for ‘F— the Jews’ video defends himself on antisemitic podcast
In Case You Missed It
-

Culture How one Jewish woman fought the Nazis — and helped found a new Italian republic
-

Opinion It looks like Israel totally underestimated Trump
-

Fast Forward Betar ‘almost exclusively triggered’ former student’s detention, judge says
-

Fast Forward ‘Honey, he’s had enough of you’: Trump’s Middle East moves increasingly appear to sideline Israel
-
Shop the Forward Store
100% of profits support our journalism
Republish This Story
Please read before republishing
We’re happy to make this story available to republish for free, unless it originated with JTA, Haaretz or another publication (as indicated on the article) and as long as you follow our guidelines.
You must comply with the following:
- Credit the Forward
- Retain our pixel
- Preserve our canonical link in Google search
- Add a noindex tag in Google search
See our full guidelines for more information, and this guide for detail about canonical URLs.
To republish, copy the HTML by clicking on the yellow button to the right; it includes our tracking pixel, all paragraph styles and hyperlinks, the author byline and credit to the Forward. It does not include images; to avoid copyright violations, you must add them manually, following our guidelines. Please email us at [email protected], subject line “republish,” with any questions or to let us know what stories you’re picking up.