Should All Ashkenazi Women Get Tested for BRCA Gene Mutations?

Life-Saving Screening: A radiology technician examines a mammography test. Image by Thinkstock
No family history of cancer? Get tested anyway suggests a recently-published study, but medical experts are deeply divided.
The study indicates that even Ashkenazi women with no family history of the disease but who test positive for a cancer-causing genetic mutation have high rates of breast and ovarian cancer.
At the heart of the dispute is the question of whether all women of Ashkenazi Jewish descent should now get genetic testing to determine if they have the mutations of the BRCA1 or BRCA2 gene. And, if they do get tested, what should they do if the results show mutations?
Ashkenazim are at a particularly high risk for these mutations: One in 40 carries a BRCA mutation as compared to one in 345 in the general population. But until now, the United States Preventive Services Task Force has recommended against routine genetic counseling or BRCA testing for women who had no family history of cancer.
Citing their findings, published September 5 on the website of the Proceedings of the National Academy of Sciences, the study’s authors recommended routine screening of all women of Ashkenazi backgrounds for harmful mutations in the BRCA genes. Some prominent experts agree.
“I think it is going to be a game changer,” said Dr. Harry Ostrer, a noted geneticist at the Albert Einstein College of Medicine, in New York, referring to the study results. “I think it puts the U.S. Preventive Services Task Force on notice.”
Ostrer said he had just returned from a bar mitzvah, where the study was making waves. “People were walking up to me and saying, ‘Gee, I want to be tested. How do I do that?” he said.
Some genetics experts, however, pointed to the limited size of the sample and a perceived dearth of broader studies that would support changing the protocol for whom to test. Among the skeptics were Dr. Mary Daly, chair of the Department of Clinical Genetics at Fox Chase Cancer Center. “Can we actually extrapolate the findings from this — from what was a relatively small and very selected study in a very select population to other populations?” she asked.
The study, conducted on a sample of 211 Ashkenazi Jewish women in Israel who were BRCA mutation carriers, found that some 60% of BRCA1 carriers and one-third of BRCA2 carriers developed breast or ovarian cancer by age 60, including many women with no history of these cancers in their families. By the age of 80, the percentage of women developing these cancers rose to 83% and 76%, respectively.
The American Cancer Society, the nation’s largest organization dedicated to supporting and interpreting cancer research, has not yet taken a clear stand in reaction to the study. Dr. J. Leonard Lichtenfeld, the society’s deputy chief medical officer, called the study “thought provoking” in a New York Times interview. However, he said that routine screening for BRCA mutations had “not been on the table” in the United States and would have to be discussed extensively and in great detail.
The current standard for screening women in the United States for cancer-causing genetic mutations is to test only those who have a high incidence of breast or ovarian cancer in their family. The study’s researchers, including its lead author, Dr. Ephrat Levy-Lahad, director of the Medical Genetics Institute at Shaare Zedek Medical Center, in Jerusalem, argue that routine testing of Ashkenazim would uncover many BRCA mutation carriers who otherwise would never learn they are at an increased risk for breast and ovarian cancer.
Ostrer compared BRCA-carrier testing to other, more common tests, pointing out that 2% of the population consists of mutation carriers, a figure in the range of cystic fibrosis and Tay-Sachs disease, which people commonly get tested for before having children. “I am sure there will be a lot of pressure to also test for BRCA1 and 2, which will have a more measurable impact because you need only one mutation to develop breast cancer. The two mutations that are required for Tay-Sachs make the disease less common,” he said.
Dr. Olufunmilayo Olopade, director of The Center for Clinical Cancer Genetics and Global Health, at the University of Chicago, said the idea of screening all Ashkenazi Jewish women was long overdue. “I am a medical oncologist and tired of waiting for people to get cancer and then get genetic testing,” she said. “We now have better tests to identify women with BRCA mutations in the population, and we should now focus on more effective ways to prevent cancer in such women.”
But Dr. David Fishman, director of the Mount Sinai Ovarian Cancer Risk Assessment Program, pointed to the gravity of testing positive for a mutation and contending with the question of whether to have preventive surgery such as the removal of breasts, ovaries and fallopian tubes. In addition, 3% of those with breast cancer are male. For that reason, Fishman said, the testing could not be restricted to women. “Is a man going to have prophylactic breast surgery? What do you do with the test results?” he asked.
The study’s researchers screened more than 8,000 healthy Ashkenazi Jewish men 30 and older for one of three BRCA mutations, in effect isolating a group that was not weighted toward families with a history of breast and ovarian cancer. Of that group, 175 men were determined to carry one of the mutations. The researchers then tested female relatives of the men who carried mutations, finding the 211 women who were carriers. Half reported little or no family history of cancer.
Despite that lack of family history, many of the women in this smaller group developed cancer.
Yet Daly questioned whether those findings would be validated in United States. “I suspect the Ashkenazi Jewish population in Israel is quite different than in any other country where there is probably a lot of other mixtures of genes,” she said.
Fishman went further, saying that even isolating whom to test would be a mammoth task. “Some people are adopted, so they don’t know their family history; some people don’t know that their family were Jews at one point. Most people don’t have a clue if they are Ashkenazi or not. And what about all the people who think they might be Jewish?” he asked.
Patient advocates shied away from weighing in on the debate, instead focusing on the complexity of genetic testing and its implications. Sue Friedman, executive director of FORCE: Facing Our Risk of Cancer Empowered said, “We strongly encourage anyone who is considering BRCA testing to begin by meeting with a qualified genetics expert prior to and after undergoing genetic testing so that they can make informed decisions about their health care.”
Elana Silber of Sharsheret, which supports Jewish families contending with breast cancer, agreed. “The study pushes further the public debate over the benefits of population wide genetic testing, and underscores the very personal questions that Jewish families must be prepared to address,” she said. All cited the critical need for people to see a genetics counselor to make informed decisions about their health.
Contact Karen Iris Tucker at [email protected]
The Forward is free to read, but it isn’t free to produce

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward.
Now more than ever, American Jews need independent news they can trust, with reporting driven by truth, not ideology. We serve you, not any ideological agenda.
At a time when other newsrooms are closing or cutting back, the Forward has removed its paywall and invested additional resources to report on the ground from Israel and around the U.S. on the impact of the war, rising antisemitism and polarized discourse.
This is a great time to support independent Jewish journalism you rely on. Make a gift today!
— Rachel Fishman Feddersen, Publisher and CEO
Support our mission to tell the Jewish story fully and fairly.
Most Popular
- 1

Culture Cardinals are Catholic, not Jewish — so why do they all wear yarmulkes?
- 2

Fast Forward Ye debuts ‘Heil Hitler’ music video that includes a sample of a Hitler speech
- 3

News School Israel trip turns ‘terrifying’ for LA students attacked by Israeli teens
- 4
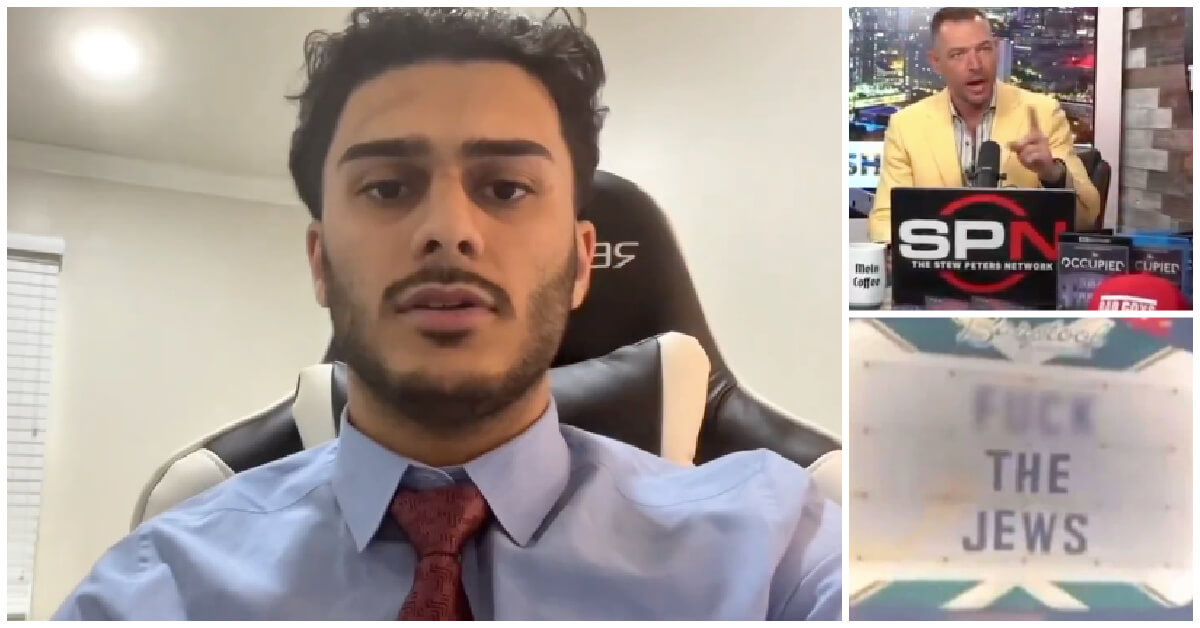
Fast Forward Student suspended for ‘F— the Jews’ video defends himself on antisemitic podcast
In Case You Missed It
-

Yiddish קאָנצערט לכּבֿוד דעם ייִדישן שרײַבער און רעדאַקטאָר באָריס סאַנדלערConcert honoring Yiddish writer and editor Boris Sandler
דער בעל־שׂימחה האָט יאָרן לאַנג געדינט ווי דער רעדאַקטאָר פֿונעם ייִדישן פֿאָרווערטס.
-

Fast Forward Trump’s new pick for surgeon general blames the Nazis for pesticides on our food
-
Fast Forward Jewish feud over Trump escalates with open letter in The New York Times
-

Fast Forward First American pope, Leo XIV, studied under a leader in Jewish-Catholic relations
-
Shop the Forward Store
100% of profits support our journalism
Republish This Story
Please read before republishing
We’re happy to make this story available to republish for free, unless it originated with JTA, Haaretz or another publication (as indicated on the article) and as long as you follow our guidelines.
You must comply with the following:
- Credit the Forward
- Retain our pixel
- Preserve our canonical link in Google search
- Add a noindex tag in Google search
See our full guidelines for more information, and this guide for detail about canonical URLs.
To republish, copy the HTML by clicking on the yellow button to the right; it includes our tracking pixel, all paragraph styles and hyperlinks, the author byline and credit to the Forward. It does not include images; to avoid copyright violations, you must add them manually, following our guidelines. Please email us at [email protected], subject line “republish,” with any questions or to let us know what stories you’re picking up.