What Little I Know About Medicine
I thought I would title this month’s column “What I Don’t Know About Medicine,” but my editors want 800 words, not an encyclopedia. What I do know about medicine should fit nicely into the space allotted.
The rotation I’m starting this week is known in hospital jargon as the sub-internship; the registrar’s office calls it “advanced medicine.” In this rotation the medical student plays the role of an intern, a first-year resident. He can write orders on the computer, decide on a course of treatment and prescribe medications — all with the co-signature of a supervisor, of course. The main thing is that the student manages his own list of patients. In other words, I won’t be following a resident around anymore; I will be a resident.
More precisely, I’ll be pretending to be a resident. That’s the catch of this rotation — it’s the adolescence of medical education, in which one is something more than a senior student but something less than an intern. How much like an intern will I be? If one reasons by similarity of activity (lack of sleep; independent decision-making on behalf of actual patients), I could very well call myself the intern. Could I walk into my patient’s room and say, “I’m Dr. Berger, and I’ll be taking care of you during your stay in the hospital?” The second half of this statement is definitely true, but the first part (with “Dr.”) isn’t quite. I won’t have my medical degree until my graduation in May 2006, and I won’t have a license to practice medicine until I finish my boards, which stretch from now (while I’m still a medical student) until the end of my residency.
On this rotation, I don’t plan to introduce myself as “Doctor” (that would be quite a stretch), but I understand why some of my colleagues would. While many patients don’t understand the difference between senior medical students, interns, residents, fellows and attending physicians, they come to appreciate something of the hierarchy during their hospital stay. One thing soon becomes clear to them: Medical students are at the bottom of the totem pole of health care providers. (Or almost at the bottom —more on that subject, below.) If a sub-intern walks into a patient’s room and starts out by saying, “My name’s Joseph Brighteyes, I’m a medical student, and I’m here to take care of you,” the patient is likely to respond, “That’s great, Joe, but who’s going to be my doctor?”
Is qualification defined more by knowledge or by capability? This larger question comes up when talking about the thousands of people whose elbow grease makes a big hospital run as smoothly as it can. Even lower on the pole than the medical student is the physician assistant. P.A.s train for fewer years than medical students, so they often get less respect from folks in medical academia. But in every rotation where, as a medical student, I’ve worked together with P.A.s or P.A. students, they have seemed more on the ball than the medical students — not as over-theoretically concerned with fascinating disease entities and more knowledgeable about what might immediately help the patient. Part of the reason is that the P.A. student spends more time in her early training (most P.A.s I’ve met are women) familiarizing herself with the way things actually are in the uncompromisingly practical universe of the hospital or clinic. Perhaps P.A.s can’t name 12 different kinds of small-vessel disease. (I’m making up that number; I certainly can’t name them, either — not off the top of my head.) But such encyclopedic knowledge is sometimes transcended, or rendered irrelevant, by practical considerations. On the other hand, you don’t want to miss the rare diseases when they do pop up. So both kinds of training (practical and theoretical encyclopedic) are essential, even complementary. The trick is to appreciate both kinds of thinking at the same time, even though most people find one of them more congenial than the other.
A similar divide is evident in the Jewish tradition, especially with regard to Torah study. In previous generations — and even today in some circles — memorizing vast tracts of the Talmud is a prized skill. On the other hand, if you’ve dipped into any of the Talmud, you know that it takes considerable exegetical ingenuity to derive laws applicable to everyday life from the rich stew of magic, folklore, intellectual speculation, casual yeshiva talk and campfire tales about the destroyed Temple. (Even the strict constructionists, those who actually bury their fingernail clippings according to the magical practice of the rabbis, still have to exercise creativity in deriving everyday religious practice from Babylonian-Jewish digression.) The two skills — encyclopedic knowledge of the Talmud and the ability to apply the Talmud to everyday religious life — are complementary, but rarely are found in the same person. Many of the greatest talmudic scholars have famously refused to adjudicate Jewish law, protesting that they could see all sides of any issue.
Today’s Jewish communities rely very much on what some people call “para-rabbis” — people who aren’t religious scholars but are reliable, even expert, in the details of daily practice. You might have met some of them: the guy who knows everything about building a sukkah; the woman who is obsessed with reading Torah; the member of the local synagogue who knows exactly how to help a recently bereaved family.
In other words, Jews (at least religious Jews) depend on “rabbis’ assistants.” In the same way, a hospital must cobble together a vast number of people who have different abilities. Some sit in offices and absorb themselves in the study of disorders affecting 10 people in the entire world, while others, down amid the gore in the E.R., can contradict those same scholars with absolute certainty if they see in front of them a practical problem they know how to solve quickly and effectively.
Bit by bit, I hope to amass both kinds of knowledge till I can be considered a doctor (a learned person, according to the word’s historical meaning) in at least one of these categories. But no matter what, there always will be plenty of material for my upcoming masterwork, “What Zack Berger Doesn’t Know.” I look forward to doing the research.
Zackary Sholem Berger is becoming a doctor, hour by sleepless hour. Feel free to write him about it at [email protected].
The Forward is free to read, but it isn’t free to produce

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward.
Now more than ever, American Jews need independent news they can trust, with reporting driven by truth, not ideology. We serve you, not any ideological agenda.
At a time when other newsrooms are closing or cutting back, the Forward has removed its paywall and invested additional resources to report on the ground from Israel and around the U.S. on the impact of the war, rising antisemitism and polarized discourse.
This is a great time to support independent Jewish journalism you rely on. Make a gift today!
— Rachel Fishman Feddersen, Publisher and CEO
Support our mission to tell the Jewish story fully and fairly.
Most Popular
- 1

Fast Forward Ye debuts ‘Heil Hitler’ music video that includes a sample of a Hitler speech
- 2

Opinion It looks like Israel totally underestimated Trump
- 3

Culture Cardinals are Catholic, not Jewish — so why do they all wear yarmulkes?
- 4
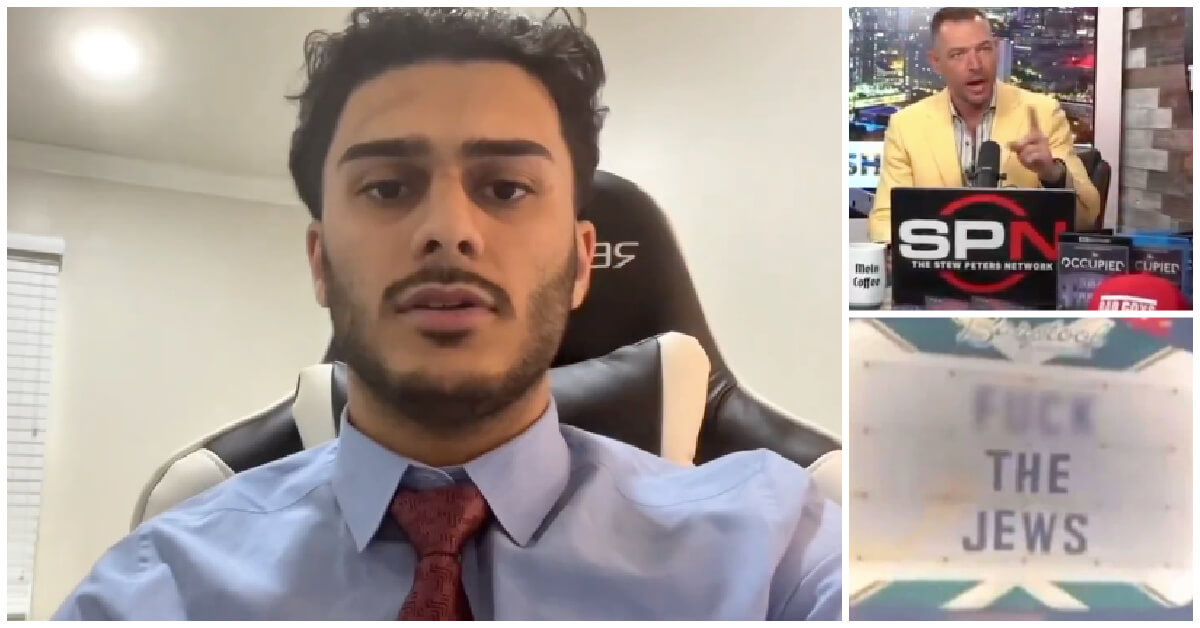
Fast Forward Student suspended for ‘F— the Jews’ video defends himself on antisemitic podcast
In Case You Missed It
-

Culture Should Diaspora Jews be buried in Israel? A rabbi responds
-

Fast Forward In first Sunday address, Pope Leo XIV calls for ceasefire in Gaza, release of hostages
-
Fast Forward Huckabee denies rift between Netanyahu and Trump as US actions in Middle East appear to leave out Israel
-

Fast Forward Federal security grants to synagogues are resuming after two-month Trump freeze
-
Shop the Forward Store
100% of profits support our journalism
Republish This Story
Please read before republishing
We’re happy to make this story available to republish for free, unless it originated with JTA, Haaretz or another publication (as indicated on the article) and as long as you follow our guidelines.
You must comply with the following:
- Credit the Forward
- Retain our pixel
- Preserve our canonical link in Google search
- Add a noindex tag in Google search
See our full guidelines for more information, and this guide for detail about canonical URLs.
To republish, copy the HTML by clicking on the yellow button to the right; it includes our tracking pixel, all paragraph styles and hyperlinks, the author byline and credit to the Forward. It does not include images; to avoid copyright violations, you must add them manually, following our guidelines. Please email us at [email protected], subject line “republish,” with any questions or to let us know what stories you’re picking up.