Farewell to a Mom’s Haven
The oldest birthing center in the country just closed. And I’m bereft.
The Elizabeth Seton Childbearing Center, aka the ESCbC, was the focus of my life when Josie was teeny. Back when I was sleepless and isolated and convinced that I was accidentally going to drown my unearthly slippery infant in the tub because I was the most inept parent who ever walked the earth, ESCbC gave me comfort and community.
No matter how bad things got, I knew I could wheel the Josinator over to West 14th Street for new-mom support groups, CPR classes, infant massage lessons, how-to-wangle-that-infernal-sling workshops. I didn’t give birth at ESCbC, but I learned a lot about how to be a mom there. And I hoped that when it came time for Josie to have a sibling, God willing, that new little person would enter the world in one of Elizabeth Seton’s comfy birthing suites. My hypothetical spawn-to-be would have joined the 3,000 babies delivered by the Seton midwives over the past three decades. (Maybe even under water! In one of Seton’s big ol’ Jacuzzi tubs! Because I am a hippie!)
Back when I got pregnant, I didn’t know a lot of people in New York with babies. At ESCbC, I met the women who are now my mom-buddies. Though some of us are back at work and others are staying home, we still e-mail and hang out, and our kids are now old enough to play together. “If any of you ever called and said, ‘I need help,’ I would be there in a heartbeat,” my Seton friend Shannon said. “There’s a sense of community at Elizabeth Seton, and that’s what’s so devastating about its loss. A support system is what makes a happy, healthy family and a strong community.”
So why did the center have to close after nearly 30 years serving the women of New York? Because it could no longer afford malpractice insurance. “On July 10, we got notice that our insurance carrier wasn’t renewing our policy,” said Kristen Stehle, a nurse practitioner at the center. “At first it didn’t seem like an emergency,” she told me. “Management looked at other carriers for different options, but they quickly learned that the lowest premium for a year — for less coverage than we’d had — was $1.2 million. For the previous year it had been $460,000.”
Ironically, giving birth at Elizabeth Seton was probably both safer and cheaper than having a baby at a hospital. ESCbC’s caesarean section rate was only 10%, far lower than the national rate of 26%. Ninety-nine percent of ESCbC’s clients were breast-feeding by the time they left the center, compared to 67% nursing when discharged from the hospital. (The surgeon general’s goal is to have 75% of women nursing at discharge.) Nursing has huge long-term health benefits for both mother and child. And a study in the June 2003 issue of the American Journal of Public Health found that women who received collaborative midwifery care (meaning care in which midwives handle most of the work and physicians are called in if there are complications) had birth-success rates (meaning healthy babies delivered at term to healthy moms) comparable to those who saw only physicians — but at a far lower cost to the health-care system. The moms spent less time in the birthing center or hospital, had fewer episiotomies and fewer technical interventions. How unfortunate, then, that a midwifery center, which ultimately saves society money, can’t afford to stay open.
This is a national crisis. Insurance rates for OB-GYNs as well as midwives have shot up in the past couple years, across the country. Hospitals in Pennsylvania and Arizona have discontinued their obstetrics services, and many doctors in Florida are considering avoiding services with high legal risks (such as mammogram reading), according to The Tampa Tribune. Delaware, Mississippi, Nevada, New Jersey, North Carolina, Ohio, Oregon, South Carolina, Texas, Washington and West Virginia have also been hit hard. And so has New York. The practice I used with Josie, the Soho Midwives center, closed several months before Elizabeth Seton did, for the same reason.
“This is much bigger than Elizabeth Seton,” said Deanne Williams, executive director of the American College of Nurse-Midwives. “The bigger question here is: Are you going to have access to care and the kind of care you want? Every woman who’s ever had a baby knows it’s the most vulnerable, scary, life-altering time, and it’s not just a physical event. You want more than reassurance that your blood pressure’s fine and the baby’s growing. You want to be involved in the decisions about how this experience unfolds for you and your family.”
And in fact, even among obstetrics and midwifery practices that can afford to stay open, malpractice concerns affect care in ways they shouldn’t. In an earlier column, I wrote about how I felt over-tested and over-medicalized during my pregnancy, even in a midwifery practice. My suspicion that all those procedures, which turned me into a nervous khaleria, were primarily “CYA tests” (that’s medicalese for Cover Your Tukhes, in loose translation) was corroborated by a recent Harris Interactive poll. Of 300 physicians surveyed, 76% felt that concern about malpractice suits was hurting their ability to provide quality care, and 94% felt that extra tests, referrals and procedures resulting from their fear of liability contributed in a significant way to health-care costs.
Look, it’s clear we need major malpractice insurance reform. I encourage everybody to urge their elected officials to take action and to vote for candidates who’ll work for serious changes in our health-care system. But none of that will bring back the Elizabeth Seton Childbearing Center, where I found friendship and sisterhood and the feeling that I wasn’t alone. At ESCbC I swapped strategies for introducing bottles, getting Josie to sleep through the night, coping with breast infections and dealing with marital stresses caused by this new little person. Shannon says, “I honestly think that if there were an Elizabeth Seton for every community, there wouldn’t be child abuse.” Maybe I wouldn’t go that far, but I do know that whenever women’s choices about where and how to give birth are restricted, we all suffer. And whenever we lose a community hub, we’re all a little lonelier for it.
Write to Marjorie at [email protected].
The Forward is free to read, but it isn’t free to produce

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward.
Now more than ever, American Jews need independent news they can trust, with reporting driven by truth, not ideology. We serve you, not any ideological agenda.
At a time when other newsrooms are closing or cutting back, the Forward has removed its paywall and invested additional resources to report on the ground from Israel and around the U.S. on the impact of the war, rising antisemitism and polarized discourse.
This is a great time to support independent Jewish journalism you rely on. Make a gift today!
— Rachel Fishman Feddersen, Publisher and CEO
Support our mission to tell the Jewish story fully and fairly.
Most Popular
- 1

Fast Forward Ye debuts ‘Heil Hitler’ music video that includes a sample of a Hitler speech
- 2

Opinion It looks like Israel totally underestimated Trump
- 3

Culture Cardinals are Catholic, not Jewish — so why do they all wear yarmulkes?
- 4
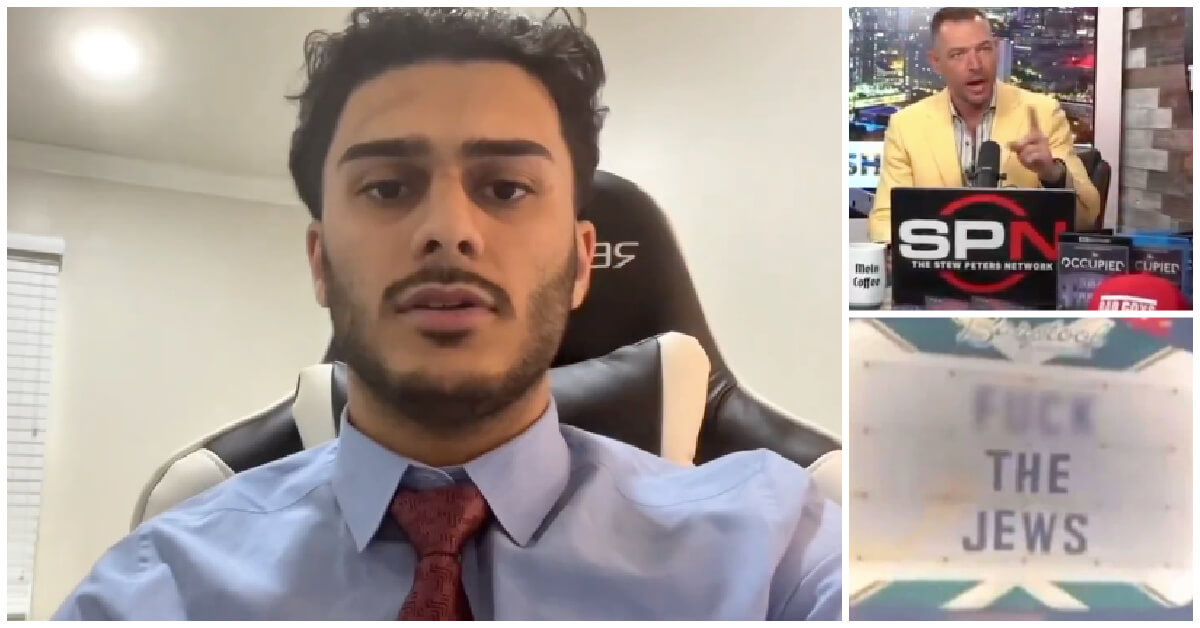
Fast Forward Student suspended for ‘F— the Jews’ video defends himself on antisemitic podcast
In Case You Missed It
-

Fast Forward In first Sunday address, Pope Leo XIV calls for ceasefire in Gaza, release of hostages
-
Fast Forward Huckabee denies rift between Netanyahu and Trump as US actions in Middle East appear to leave out Israel
-

Fast Forward Federal security grants to synagogues are resuming after two-month Trump freeze
-
Fast Forward NY state budget weakens yeshiva oversight in blow to secular education advocates
-
Shop the Forward Store
100% of profits support our journalism
Republish This Story
Please read before republishing
We’re happy to make this story available to republish for free, unless it originated with JTA, Haaretz or another publication (as indicated on the article) and as long as you follow our guidelines.
You must comply with the following:
- Credit the Forward
- Retain our pixel
- Preserve our canonical link in Google search
- Add a noindex tag in Google search
See our full guidelines for more information, and this guide for detail about canonical URLs.
To republish, copy the HTML by clicking on the yellow button to the right; it includes our tracking pixel, all paragraph styles and hyperlinks, the author byline and credit to the Forward. It does not include images; to avoid copyright violations, you must add them manually, following our guidelines. Please email us at [email protected], subject line “republish,” with any questions or to let us know what stories you’re picking up.