Can New Study on Binge Eating Disorder Explain Intergenerational Holocaust Trauma?

Graphic by Angelie Zaslavsky
This article originally appeared in the Yiddish Forverts.
A strand of DNA is a lot like computer software; it’s the blueprint for the complex computations that cells perform, and like a coding error in a computer program, a single mutation—either a deletion, insertion, or duplication—to the strand can cause cells to malfunction. But DNA doesn’t do all the work on its own. Just as a computer needs to be turned on for its software to run, genes are frequently switched on and off by the environment. This phenomenon is known as epigenetics.
At the Weizmann Institute in Rehovot, Israel, scientists studying the neurobiology of stress have published a new report suggesting that the development of certain psychiatric diseases may be pre-programmed into us in the womb in response to a challenging environment. The study, published online on June 1 in the journal Cell, is the first to demonstrate a mechanistic link between epigenetics and the development of psychiatric disease and may have particular relevance for the Jewish community.
The team of scientists was interested in how exposure to stress during pregnancy could put the developing fetus at a greater risk of developing Binge Eating Disorder, a psychiatric disease that causes frequent consumption of large amounts of caloric foods in short periods of time.

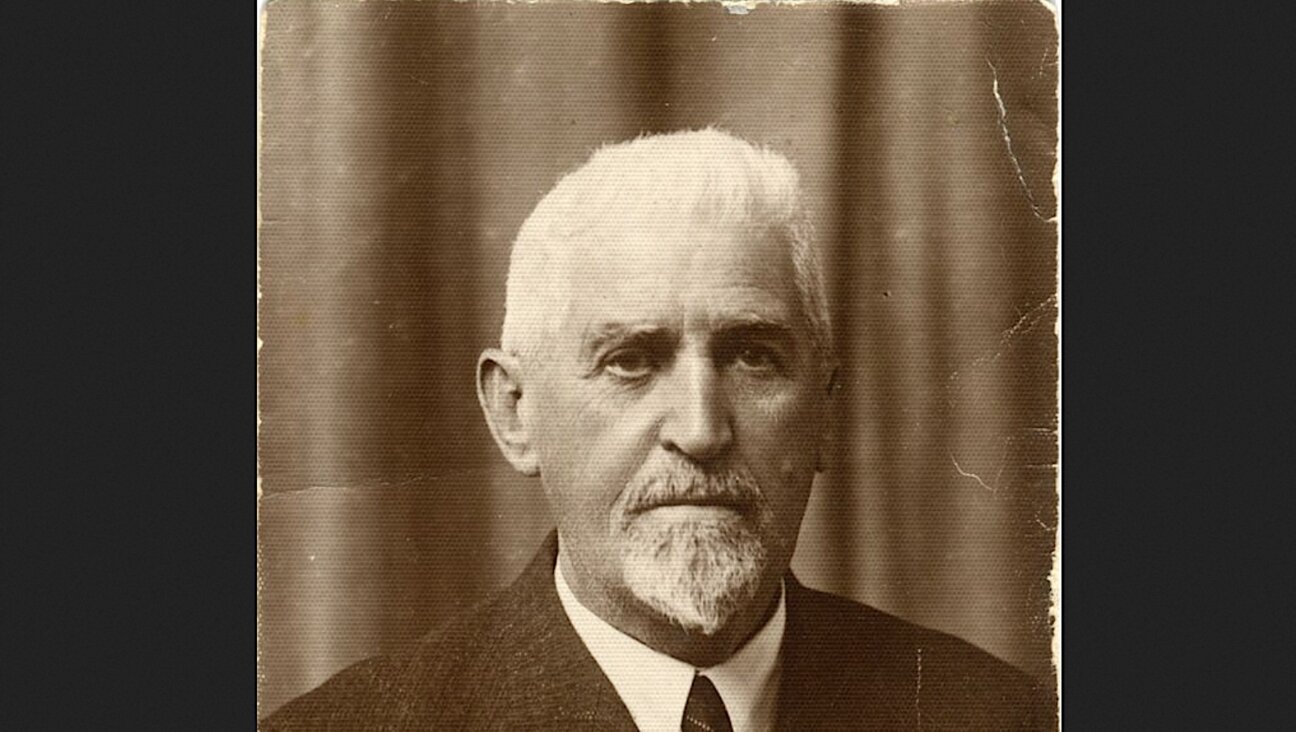
Dr. Alon Chen, the lead researcher of the study at the Weizmann Institute in Rehovot
“Although eating disorders are known to be epigenetically linked with stress exposure, nothing is known about the underlying mechanisms,” Dr. Alon Chen, the lead researcher of the study, said. “For the first time, we demonstrated a mechanistic link between prenatal stress and increased susceptibility to eating disorders.”
According to statistics from the National Institute of Health, Binge Eating Disorder is most prevalent in Western countries, where foods tend to be the most caloric. In the United States, an estimated 3% of women and 2% of men suffer from the disease.
Binge Eating Disorder can be life-threatening: those affected by it are more likely to be obese and are at a significantly greater risk of developing diabetes, high cholesterol, and cardiac problems. Currently, there is only one FDA-approved drug for treating the disorder; it’s expensive and risky, as users can build up a tolerance to it. While psychotherapy, antidepressants, and epilepsy medications can help, they are far from ideal. And since the effects of the disorder are long-term, insurance companies are less likely to cover treatment.
To mimic the effects of a stressful environment, the researchers gave pregnant mice a drug that caused them to produce more corticosterone, a hormone that’s released in the brain in response to stress. During pregnancy, as corticosterone levels increase, the fetus receives fewer nutrients through the placenta. According to the theory of evolution, this mechanism is beneficial to mice as it enables the mother to program her developing fetus to slow down its metabolism in preparation for an environment where food is scarce. But what happens if these pre-programmed offspring are born into an environment rich in caloric foods?
The result was clear. When the adult offspring of mice exposed to maternal stress were fed a “Western” diet high in calories over short periods of time, the females displayed symptoms of Binge Eating Disorder.
The researchers then repeated the same experiment, but this time, they examined the prenatal brains of the female offspring. When they looked at the hypothalamus, a region of the brain involved in metabolic processes as well as response to stress, they found that maternal stress had reduced the expression levels of a class of genes called methyltransferases that are critical for normal cognitive function, including regulation of stress.
In other words, the environment had triggered cells to switch off these genes.
“We discovered a very interesting thing,” Chen said. “Looking at embryos’ brains, we saw large molecular differences between offspring whose mothers’ stress mechanism was activated and those in whose mothers it was not activated. However, in adulthood, the differences disappear. The differences will be expressed only when the mice are exposed to some form of challenge. This signifies that an epigenetic, rather than a genetic, marker was introduced at the embryonic stage as there was no change in the genes.”
But for Chen and his team, this was hardly the most surprising finding. When the scientists provided the mice with Binge Eating Disorder a diet that was rich in certain nutrients such as vitamins B12 and B6, they were able to reverse the effects of the disorder.
“We succeeded in preventing the disorder from emerging simply by providing a balanced diet,” Chen said.
He believes that humans have a similar mechanism for transmitting information about the environment to the developing fetus. “All the biological genes and pathways described are shared by mice and humans,” he explained.
For the Jewish community these findings may be especially relevant. In the last few years, new research has suggested that Holocaust trauma can be transmitted intergenerationally through epigenetic modifications. In 2015, scientists at Mount Sinai Hospital in New York found that the children of Holocaust survivors expressed higher levels of a gene associated with post-traumatic stress disorder, compared to Jews whose parents lived outside of Europe during World War II.
According to Dr. Moshe Szyf, a professor of pharmacology and therapeutics at McGill University who specializes in epigenetics, Chen and his team’s results suggest that epigenetic transmission of Holocaust trauma may have occurred as early as pregnancy or early childhood.
But given that the trauma occurred mostly prior to pregnancy, how might it have been transmitted to the next generation?
“The most probable transmission is through maternal behavior, which was ‘reprogrammed’ by the mother [as a result] of previous exposure to trauma,” Dr. Szyf explained. He believes that exposure to maternal trauma may have activated the release of stress hormones that could turn on and off genes regulating trauma.
For now, the following question remains to be answered: Can diet alone reverse or alleviate the symptoms of stress-related psychiatric diseases such as eating disorders and Post Traumatic Stress Disorder? Chen says it’s “hard to predict but reasonable to suggest that part of the epigenetic signature,” that is, the changes in gene expression, “could be modified by a relevant diet.”