Could Kashrut Be Partly To Blame for Crohn’s Disease?

Image by Getty Images
Here’s a question that has puzzled scientists for decades: Why is Crohn’s disease — an inflammatory bowel disease (IBD) with the highest incidence among Caucasians — about two to four times more prevalent among Ashkenazi Jews than among non-Jewish whites?
As some researchers continue to look for the answer in our genes, others are proposing a more provocative theory that invokes factors unique to the Jewish diet and to the environment shared by Jews in recent history.
To date, more genes have been linked to Crohn’s than to any other disease. In a single paper published late last year, scientists reported finding 30 new genes associated with Crohn’s, bringing the total of such genes up to 71. (Ulcerative colitis, the other common IBD, isn’t far behind, with 47 genes.)
To determine whether genetics could explain the higher incidence of Crohn’s among Ashkenazi Jews, a team led by Dr. Robert Desnick, dean of genetics and genomic sciences at the Mount Sinai School of Medicine in New York, tested for 22 mutations across 10 of the most established Crohn’s-related genes in nearly 900 Ashkenazi Jews, both with the disease and without.
To the team’s surprise, the mutations found in this group of Jewish subjects were as common and had as great an impact as they did among non-Jews in previous studies.
“What we learned is that there is no difference,” said Desnick, who reported the findings in June in the journal BMC Medical Genetics. “So it has to be something else.”
One possibility is that mutations in some of the other disease-associated genes not tested in Desnick’s study are at higher frequencies among Ashkenazi Jews, or that mutations specific to this community haven’t yet been found. Indeed, the Mount Sinai team discovered two novel mutations in their study, and they are now looking for more, according to the study’s lead author, Inga Peter, a professor of genetics and genomic sciences at the school.
But some researchers contend that science should be looking outside our genes to the environment.
“It doesn’t surprise me that they didn’t find anything in the genes,” said Dr. Joel Weinstock, chief of the division of gastroenterology and hepatology at the Tufts Medical Center. “I think IBD is 90% environmental and 10% genetic.”
Crohn’s disease and colitis were virtually unheard of before the 20th century, and even today they are still quite rare in the developing world. As such, many experts believe the “hygiene hypothesis” — the idea that, absent sufficient exposure to microbes and parasites, the immune system goes awry and starts attacking the body — could be at play in these diseases.
Specifically, Weinstock has his eye on parasitic worms called helminths — which is where kashrut and Jewish history enter the picture. According to Weinstock, up through the 1930s, most people had helminths in their guts through contact with animals and contaminated water and food, including pork.
The fact that Jews coming to the United States at the turn of the century were not eating pig products, already adhered to certain cleansing rituals and tended to settle in cities far from animals and animal waste might just have been the perfect mix to set them on a path to their current Crohn’s rates. Weinstock believes that as sanitation improves around the world, other populations will develop IBD at similar rates.
A number of researchers are sympathetic to this line of reasoning. “I think it’s quite plausible,” said Dr. Judy Cho, director of the Inflammatory Bowel Disease Center at the Yale University School of Medicine.
But other experts are wary of connections to kashrut or any other cultural practices. “I think this is highly speculative, and I just don’t buy it,” said Dr. Herbert Virgin, head of pathology and immunology at the Washington University School of Medicine in St. Louis and co-chair of the Crohn’s & Colitis Foundation of America’s Genetics Initiative.
Virgin argues that genetics is still the most probable cause of the Jewish community’s vulnerability to the disease — researchers just haven’t found the mutations yet.
“Kosher practices have been observed for centuries,” Virgin said, “but the uptick in Crohn’s incidence across the Western world is much more recent.”
Contact Talia Bloch at [email protected]
The Forward is free to read, but it isn’t free to produce

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward.
Now more than ever, American Jews need independent news they can trust, with reporting driven by truth, not ideology. We serve you, not any ideological agenda.
At a time when other newsrooms are closing or cutting back, the Forward has removed its paywall and invested additional resources to report on the ground from Israel and around the U.S. on the impact of the war, rising antisemitism and polarized discourse.
This is a great time to support independent Jewish journalism you rely on. Make a Passover gift today!
— Rachel Fishman Feddersen, Publisher and CEO
Most Popular
- 1

News Student protesters being deported are not ‘martyrs and heroes,’ says former antisemitism envoy
- 2

News Who is Alan Garber, the Jewish Harvard president who stood up to Trump over antisemitism?
- 3

Fast Forward Suspected arsonist intended to beat Gov. Josh Shapiro with a sledgehammer, investigators say
- 4
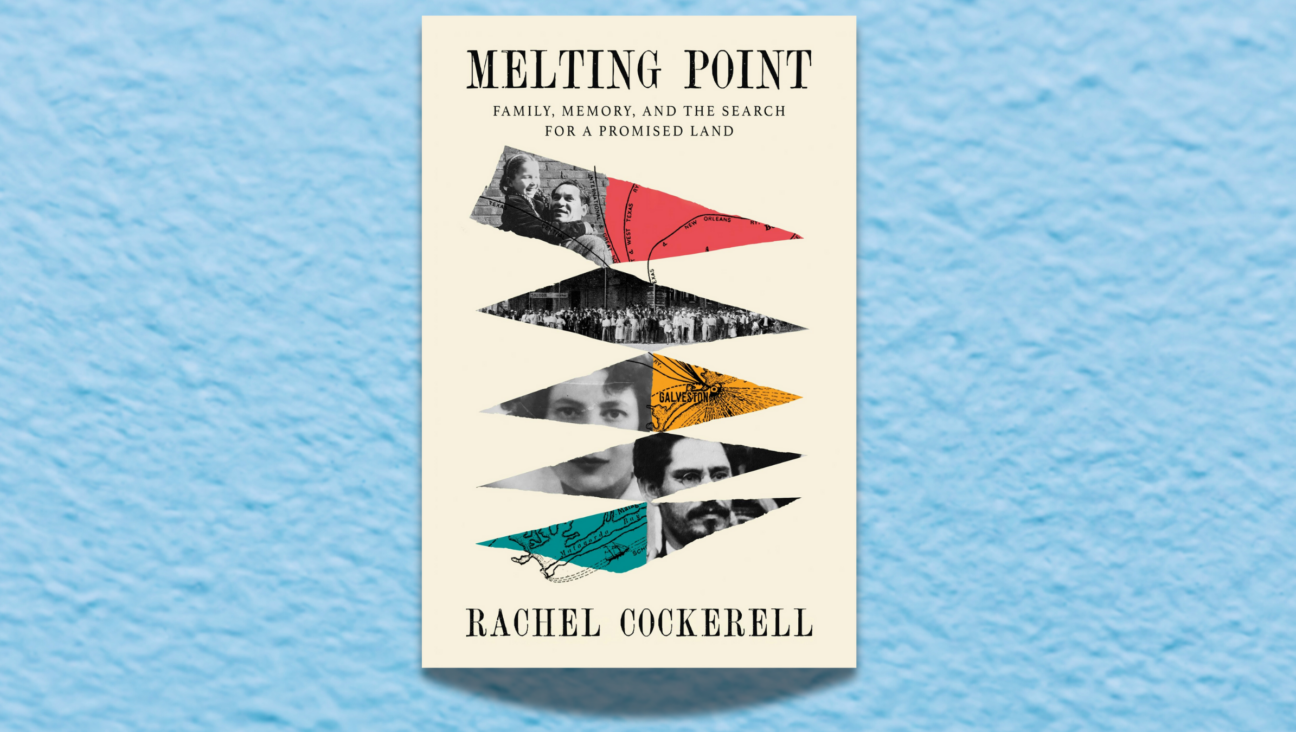
Politics Meet America’s potential first Jewish second family: Josh Shapiro, Lori, and their 4 kids
In Case You Missed It
-

Opinion Why can Harvard stand up to Trump? Because it didn’t give in to pro-Palestinian student protests
-

Culture How an Israeli dance company shaped a Catholic school boy’s life
-

Fast Forward Brooklyn event with Itamar Ben-Gvir cancelled days before Israeli far-right minister’s US trip
-

Culture How Abraham Lincoln in a kippah wound up making a $250,000 deal on ‘Shark Tank’
-
Shop the Forward Store
100% of profits support our journalism
Republish This Story
Please read before republishing
We’re happy to make this story available to republish for free, unless it originated with JTA, Haaretz or another publication (as indicated on the article) and as long as you follow our guidelines.
You must comply with the following:
- Credit the Forward
- Retain our pixel
- Preserve our canonical link in Google search
- Add a noindex tag in Google search
See our full guidelines for more information, and this guide for detail about canonical URLs.
To republish, copy the HTML by clicking on the yellow button to the right; it includes our tracking pixel, all paragraph styles and hyperlinks, the author byline and credit to the Forward. It does not include images; to avoid copyright violations, you must add them manually, following our guidelines. Please email us at [email protected], subject line “republish,” with any questions or to let us know what stories you’re picking up.