Do Orthodox Jews Need Their Own Eating Disorder Programs?

Young woman struggling with eating disorder Image by iStock
“Airplane food. That’s what they gave me to eat while I was trying to recover from an eating disorder — airplane food. For 10 weeks! Everyone else had these normal-looking meals, and I had prepackaged stuff that looked exactly like you’d get it on a plane.”
Sitting in a busy kosher cafe in midtown Manhattan last month in a stretchy, calf-length black skirt, long-sleeve top and bright-blue glasses, Lieba Brownstein rattled off the names of the seven centers she went to for in-patient and out-patient treatment over the past six years, as well as all the ways they didn’t understand her identity as Orthodox Jew.
Now 23, and finishing her second year of graduate school for social work, Brownstein began suffering from an eating disorder around age 14. Over the years, she swerved between starving herself, binging, purging and other self-harming symptoms —- all while struggling to observe and protect her strict Jewish faith, and all the rules and rituals that dictate what and when she eats.
“At first, they just gave me PB&J or bagels and tried to call those ‘kosher’ meals. Seriously. I was like, ‘Um, I am here to recover — I need food.’” That’s when they rolled out the airplane meals. “Steamed chicken breasts and carrots, which was so restrictive-feeling. Two-and-a-half months of that — of me feeling like some exotic person at every meal.”
But it wasn’t just that, Brownstein says. She woke up 45 minutes early every day to pray, otherwise she’d be interrupted while praying, or simply looked at like she was kind of crazy, given how the praying is often accompanied by what sounds to others like mumbling. She was reprimanded for bringing a prayer book to meals (“Sorry, the prayer for after you eat is a long prayer!”), and for shuckling (ritual swaying during prayer), because it was suspected to be a compensatory behavior —- that is, a way to burn extra calories.
Phone time was restricted, and she desperately wanted to call family to wish them a Good Shabbos, but she wasn’t allowed a Friday afternoon phone call. “They didn’t let me shower before Shabbat, either, on Friday afternoon, which I obviously couldn’t do the next day, when they finally would open the bathroom,” she said.
Friday nights she would have grape juice (a substitute for wine) and challah bread, but her nutritionist didn’t account for those items in her meal plan, and “unfortunately, I was not yet at a place in my recovery where I could consume those calories without them being in my plan.”
From her inability to “carry” on Shabbos — there was no eruv (this is usually a string hung at streetlight level, outlining a short area in which it’s okay to carry vital items) — to the many holidays and fast days, Brownstein felt utterly alone as an observant Jew.
“On Saturdays, most of the patients were driven to the once-a-week art therapy, but I couldn’t go,” Brownstein said. “So I just sat there.” It even got tricky with regard to shomer negiah — not touching men — when there were group sessions that involved holding hands with the person next to you, who very well could be male.
Brownstein is hardly the only deeply religious Jew whose treatment centers didn’t understand the many ways treatment might need to be different for an Orthodox Jew.
Unfortunately, she’s one of many. A 2008 study from Toronto, published in the The American Journal of Psychiatry, found that 25% of Jewish females ages 13 to 20 reported eating disorder behaviors, compared with just 18% in other religious affiliations. The other frequently cited study (now over 20 years old) found that one in 19 Jewish girls in an Orthodox Brooklyn high school suffered from some form of eating disorder, 50% higher than the rate in the general population.
The problem is prevalent. Today, Brownstein is recovered, and once she becomes a licensed clinical social worker, she is determined to create what she hopes will be the first eating disorder treatment center just for Jewish women.
She has named her project EMET — Everyone Matters Eating Treatment.

Lieba with her twin brother Ilan Image by Lieba Brownstein
“Emet is the Hebrew word for “truth,”” she said. “I believe that successful recovery requires that you stay true to yourself — and that includes your religion, values and traditions.”
Even though in 2010 The Renfrew Center, a well-known network of eating disorder facilities, created “Jewish tracks” at their network of treatment centers, most American centers are still unprepared to handle the various needs of someone of the Orthodox faith.
“It takes knowing more than just the bare bones,” said Deborah Marton, a psychologist specializing in eating disorders in New York City. Marton is also Orthodox. “You need someone who has been trained to understand the ins and out of the various practices and rituals, so that they can both determine if a patient is, in fact, using a Jewish ritual as a disordered symptom, or if they are not.”
On an anecdotal level, the pool of potential patients for Brownstein seems large. “I went to an Orthodox college,” Brownstein said. “And I’d say there was at least one person in every single class I took with an eating disorder. And ever since I put up my website announcing my intention to start EMET, so many people have messaged me, telling me they are excited about this idea, that they need this.”
Another former patient in Brooklyn echoes that impression: “It’s not an overstatement to say that I don’t know one woman in my community who doesn’t have some form of disordered eating.”
People from every background, not just Jews, can use food to cope and communicate, says Jill Lewis, a therapist who specializes in eating disorders and recently relocated to Atlanta from New York City. She is well versed in the nuances of Orthodox traditions.
“But yes, Judaism in particular is just so surrounded by food. The week’s rhythm is dictated by it, and there’s even a weekly binge, if you will — the big Shabbos meals,” she said. (Imagine tucking into a Thanksgiving meal, every single week, says Sarah Bateman, a licensed clinical social worker at The Renfrew Center, in New York City.)
When you add in other food restrictions and rigidity, the pressure to get married and the entire matchmaking process (which often includes pointed whispers about dress size, not to mention a general hush-hush outlook about mental illnesses), you really need a therapist who has a deep knowledge of these specific burdens, Lewis says.
“Oh man, they didn’t get me at all in treatment,” said Julie Sohmer*, 26, who went to four different programs in the New York City area with the past six years. “I constantly felt like I had to defend myself and that I was choosing to do something that was religious, not disordered. When it came to something as simple as not mixing meat with dairy, for instance, they’d say ‘Yes, I know it’s a religious thing, but…’ As if it wasn’t really a big deal. Like, when the nonkosher food they’d ordered in was late, they’d sort of think I could just eat the other food in a pinch.”
When Temimah Zucker was in the hospital being treated for anorexia eight years ago, she was the only Jewish person there. “While I’d say they were sensitive overall, I still felt different and isolated,” said Zucker, who’s now 26 and a therapist at Monte Nido, an eating disorder treatment center in Manhattan, where she works to raise awareness of eating disorders in the Jewish community. “At the time I wished there had been someone who understood everything, like, how a certain holiday coming up might affect me, or something.”
The kosher issue is huge, of course, and way thornier than just steering clear of bacon. “Before I went off to in-patient treatment [in South Florida] nearly two years ago, I could tell there’d be no way they do kosher food the proper way… like the way we did in my home growing up,” said Jessica Klebner*, a 30-something mother of two in Brooklyn.
Consulting with a rabbi for eating disorder-related advice — about how to handle fast days, for example, or how to approach eating in a nonkosher facility — can be an additional burden. “I literally spent six weeks before I went in-patient trying to get a rabbi to give me the sign-off — that even though the center wasn’t going to be kosher enough, that it was okay,” Klebner said. “That rabbinical blessing was very important to my husband. I was so sick — but I just couldn’t get the okay; it was insanity.”
Not everyone thinks specially designed treatment for Orthodox Jews is the magic trick, though. Sarah Cohen*, a 34-year-old psychology graduate student in Brooklyn, suffered from an eating disorder for much of her teens and early 20s, and now firmly believes that it was only after she put her recovery first — and religion second — that she could really get better. For her, this meant that the various constraints of religious life went by the wayside for a while; she ate questionably kosher food while in various treatment centers, and she didn’t adhere to the typical Shabbat schedule. “Here’s how I see it: You only have so much emotional energy to fight, and you need to save that energy to fight the disorder. The disorder is so big. Bigger than everything — even your religion. When you’re better, you can do every single thing you want again.”
And the role of religiosity in eating disorders is so, so complicated, says Sarah Weinberger-Litman, an associate professor of psychology at Marymount Manhattan College and an associate producer of the groundbreaking 2009 film about eating disorders in the Orthodox community, “Hungry To Be Heard.” Many women who are religious and who have an eating disorder “are going to go through a bit of spiritual journey during recovery, trying to sort out where the disorder and the religiosity intersect,” she said. “Some rituals or values can be used to justify symptoms, while others can have a protective effect. In the best case, a therapist will truly understand the practice so they can begin to tease apart when an internal religious value system needs to be strengthened or when someone needs to be distanced from a punitive religious practice.”
Treatment centers like Renfrew that have Jewish programs are a great start, Weinberger-Litman notes, but in a lot of cases the only professionals who are well versed in the nuances are occasional consultants, not the everyday clinicians on site.
Finding ways to make the various rituals work for her was the key to recovery, says Hillary Waller, 34, a psychotherapist in Philadelphia who sought treatment for her eating disorder. “When Passover came around, I worked with my therapy team to write my own Haggadah [aka the Seder ‘manual’],” Waller said. “My Haggadah was all about freedom from what binds me — and how I could utilize this holiday to feel free.”
Not that every ritual has a redeeming element. Fasting days are a particularly touchy subject, whether you’re someone who binges or restricts. There are six fast days for Orthodox Jews each year, each of which are typically followed by huge meals, of course. For many women with eating disorders, a day where eating is prohibited, followed by one where you stuff yourself again with a groaning table’s worth of food, can be a powerful trigger.
While a rabbi’s take on the fasting question may vary, you’d be hard-pressed to find an eating disorder therapist who approves of fasting. Ideally, a therapist can even work with the patient’s rabbi to help bring about an understanding of the issue, Marton says. “The foundation of Judaism is your health and taking care of your body,” Lewis said. “When tradition buts up against health, health must win out.” More eating-disorder-educated rabbis will steer you back toward that tenet and give their okay to skip fasting, but there may be others who don’t know enough about eating disorders and insist on rigorous adherence to religious law.
“Religious practices can be of positive value and a helpful part of the treatment process,” said Bateman, who herself is Modern Orthodox. “But women sometimes want to use their traditions in a different way. So, if Shabbat has been challenging to you, but you do want to keep it in some way, I’d encourage you to think about what you do get out of it, and what you can do differently so you can get more of that out of it. You take what has been challenging for you and work to use it as a positive in the healing process.”
Brownstein hopes to create her own center in the next few years, starting with an outpatient program in 2022. The end goal, Brownstein says, is not just recovery, but also the formation of an evolving, authentic relationship with Judaism and your body. “For me, I learned ways to love — not dread — Shabbat. And I can appreciate how dressing modestly is meant to show me how special my body is.”
Yes, food is everywhere in Judaism, and the rules can be numerous and complex, but, Brownstein said, “being Jewish should not be an obstacle to getting the right treatment or mean that you are meant to feel ‘different’ at every meal while you’re in treatment” She’s determined to show the world that with careful guidance, you can take the religious values into your hands and mold them to your own true self — and set yourself free.
*Names have been changed for privacy.
Liz Krieger is a writer in Brooklyn. Follow her on Twitter, @kriegerliz.
The Forward is free to read, but it isn’t free to produce

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward.
Now more than ever, American Jews need independent news they can trust, with reporting driven by truth, not ideology. We serve you, not any ideological agenda.
At a time when other newsrooms are closing or cutting back, the Forward has removed its paywall and invested additional resources to report on the ground from Israel and around the U.S. on the impact of the war, rising antisemitism and polarized discourse.
This is a great time to support independent Jewish journalism you rely on. Make a gift today!
— Rachel Fishman Feddersen, Publisher and CEO
Support our mission to tell the Jewish story fully and fairly.
Most Popular
- 1

Culture Cardinals are Catholic, not Jewish — so why do they all wear yarmulkes?
- 2

News School Israel trip turns ‘terrifying’ for LA students attacked by Israeli teens
- 3

Fast Forward Ye debuts ‘Heil Hitler’ music video that includes a sample of a Hitler speech
- 4
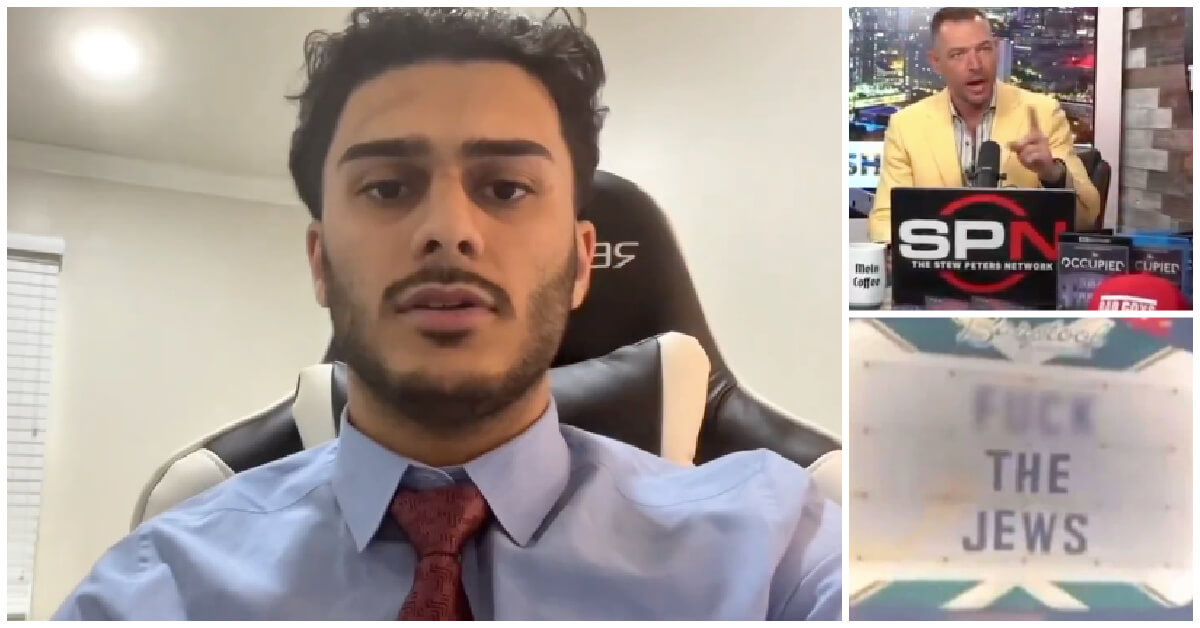
Fast Forward Student suspended for ‘F— the Jews’ video defends himself on antisemitic podcast
In Case You Missed It
-

Yiddish קאָנצערט לכּבֿוד דעם ייִדישן שרײַבער און רעדאַקטאָר באָריס סאַנדלערConcert honoring Yiddish writer and editor Boris Sandler
דער בעל־שׂימחה האָט יאָרן לאַנג געדינט ווי דער רעדאַקטאָר פֿונעם ייִדישן פֿאָרווערטס.
-

Fast Forward Trump’s new pick for surgeon general blames the Nazis for pesticides on our food
-
Fast Forward Jewish feud over Trump escalates with open letter in The New York Times
-

Fast Forward First American pope, Leo XIV, studied under a leader in Jewish-Catholic relations
-
Shop the Forward Store
100% of profits support our journalism
Republish This Story
Please read before republishing
We’re happy to make this story available to republish for free, unless it originated with JTA, Haaretz or another publication (as indicated on the article) and as long as you follow our guidelines.
You must comply with the following:
- Credit the Forward
- Retain our pixel
- Preserve our canonical link in Google search
- Add a noindex tag in Google search
See our full guidelines for more information, and this guide for detail about canonical URLs.
To republish, copy the HTML by clicking on the yellow button to the right; it includes our tracking pixel, all paragraph styles and hyperlinks, the author byline and credit to the Forward. It does not include images; to avoid copyright violations, you must add them manually, following our guidelines. Please email us at [email protected], subject line “republish,” with any questions or to let us know what stories you’re picking up.